Amit Verma (name changed on request) walked into a psychologist’s clinic convinced he was depressed. It had been months since his mother fell ill, months since a relationship ended without drama but with residue. Life was still functioning—emails sent, meetings attended—but something had dimmed. “I told my psychologist that I think I’m depressed,” Amit recalls. “I don’t feel like myself anymore,” he told her.What followed was not a rush to label. The sessions moved gently. The psychologist asked him to map his days: when the heaviness began, what seemed to trigger it, whether it ever loosened its grip. She asked about moments of relief—small, unplanned—when joy still showed up. It did. Bad days were bad, but good days still existed. His work was intact. His self-worth, bruised but not broken. After a few weeks, the conclusion surprised him. This was not depression. It was grief, quietly doing its work.Looking back, Amit can pinpoint why he couldn’t tell grief from depression. “Online, everything sounds like depression,” he says. “If you’re not sleeping well, if you feel low, if you don’t want to talk to people—there’s a label waiting for you,” adds Amit. He had been tracking intensity, not pattern. “I assumed it to be depression because it lasted for weeks,” he shares. “I didn’t realise grief can be long and still be grief because it still lets you breathe in between.”Amit’s confusion is not unusual, it is almost the default now. “The most common pattern is people using “depression” to describe situational, reactive sadness rather than a depressive disorder,” says Dr. Bhavna Barmi, chief psychologist and founder of Happiness Studio. “People confuse sadness with depression mainly because everyday language blurs the difference. ‘I’m depressed’ is commonly used to mean ‘I’m upset’. This is reinforced by low mental health literacy and social media shorthand where complex emotions get compressed into clinical labels. People aren’t taught that depression involves duration, functional impairment, and biological symptoms, not just feeling sad,” she adds. She also points to stigma as a quieter force at work, “Stigma also plays a role: Sadness is often minimized, while depression is taken seriously. So people use the term to legitimize their distress,” observes Dr. Barmi.
Language blurs the dfference.
It happens the other way round too—often more dangerously. Many people call it “just sadness” because admitting depression feels heavier than carrying it. They wait for time to fix it, for sleep to return on its own, for motivation to come back—until days start shrinking and functioning quietly collapses. In that delay, depression gets the one thing it thrives on: Silence, dressed up as normalcy.The mix-up happens because emotional pain resists neat categories. Sadness looks ordinary enough to be dismissed, yet unfamiliar enough to alarm the moment it lingers. We borrow the vocabulary available to us, and depression has become the most widely circulating word for inner distress—ready, recognisable, and oddly validating. In the absence of emotional literacy, duration replaces discernment, intensity replaces pattern, and we name what we fear rather than what we feel.
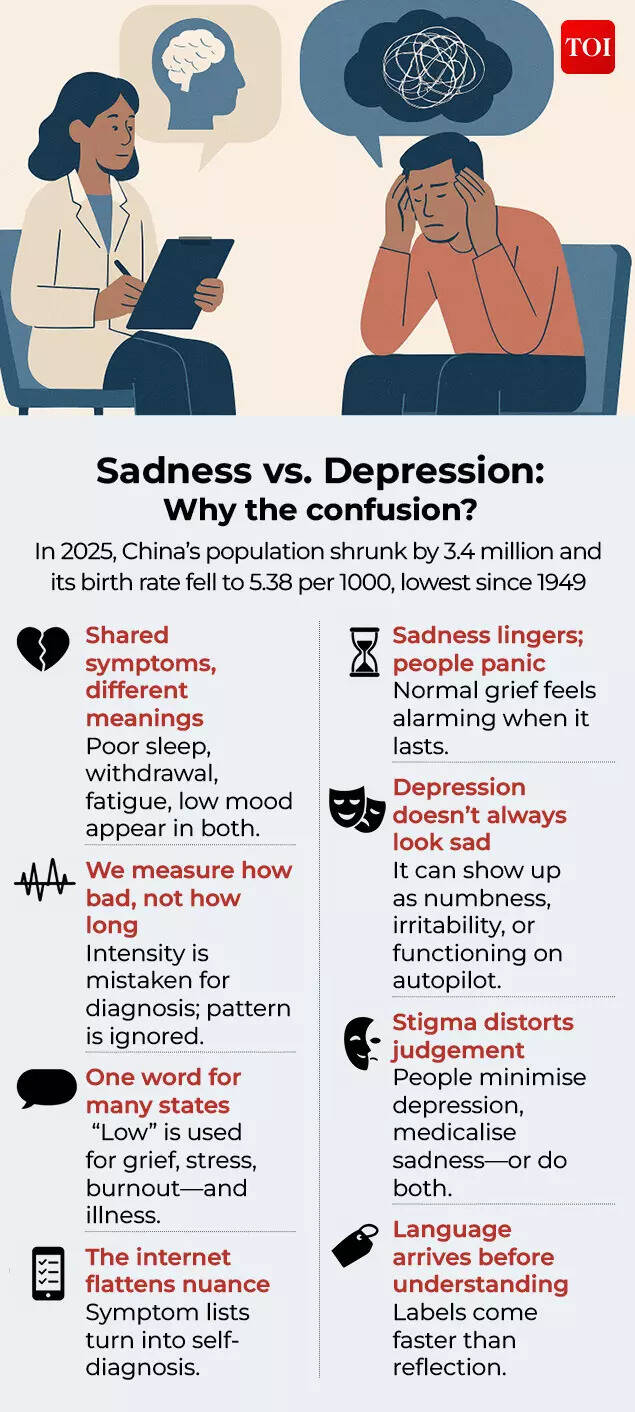
The harm lies not in the confusion itself, but in what it delays. When sadness and depression blur into one, people lose their internal compass. “When ordinary sadness is labeled as depression, people begin to see natural emotional responses to loss, failure, or stress as illness. This reduces emotional tolerance and undermines the understanding that discomfort can be meaningful, temporary, and adaptive,” reflects Dr. Barmi.Those who are grieving begin to fear they are broken, while those who are clinically depressed wait, hoping time will fix what time cannot. “People with situational sadness may seek medical solutions when what they need is support, problem-solving, or time, while those with true depression may not be taken seriously because the term has been diluted. This leads to inappropriate interventions and missed care. Perhaps the most dangerous consequence is that individuals experiencing true clinical depression may downplay their symptoms, believing they are just “going through a rough patch” or “feeling sad”. This prevents them from seeking professional help, leading to prolonged suffering and potentially more severe outcomes,” she warns.Without the language to tell one from the other, distress is either medicalised too quickly or minimised for too long. Both mistakes carry a cost. So, talking about the difference is necessary. “Openly discussing the distinction between sadness and depression is crucial because it promotes accurate self-assessment, encourages timely professional help-seeking, and helps foster a more compassionate and informed society that can provide appropriate support to those who need it. The goal is to use precise language to facilitate better mental health outcomes for everyone,” says Dr. Barmi.
Sadness and depression: When numbers draw the line
This distinction is crucial because the scale of the two states is often flattened into one. According to the Global Burden of Disease 2021 study, published in The British Journal of Psychiatry, an estimated 357 million people worldwide experienced a new episode of depressive disorder in 2021, while about 332 million were living with the condition at any given time. Even the 2025 WHO estimates keep the picture clear: About 4 per cent of the global population experience depression, including 5.7 percent of adults (4.6 per cent among men and 6.9 per cent among women).
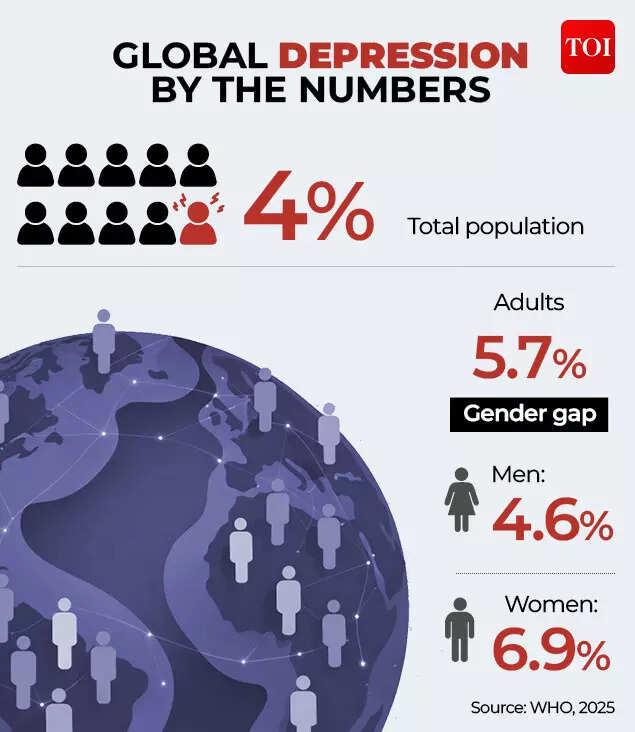
Global depression by the numbers
Depression is widespread—but it is not universal. Sadness, however, almost is. The Gallup World Poll 2024 shows that 26 percent of adults globally and 31 percent of Indians said they experienced sadness during a lot of the previous day.

How common is sadness?
That phrase is very important. “A lot of the day” does not mean a fleeting low, a bad morning, or a moment of emotional spillover. It means sadness that lingers across hours—during work, between conversations, in the quiet stretches where the mind returns to the same ache. And yet, even here, there is a crucial difference. Sadness measured this way still allows fluctuation: It can coexist with moments of relief, distraction, even competence. Depression does not hinge on how many hours a feeling lasts in a single day. It shows up as a pattern over time—shrinking energy, dulling motivation, eroding function, quietly narrowing life itself.
Sadness vs. depression: What clinicians actually mean
We often speak of sadness and depression as if they are points on the same sliding scale — one “mild”, the other “severe”. But clinicians don’t read them like that. Dr. Barmi explains that sadness is a normal, temporary human emotion that is often a reaction to specific life events like loss or disappointment, and one that fades with time. “Depression, or major depressive disorder,” she contrasts, “is a serious, diagnosable medical illness with biological, psychological, and environmental roots that causes pervasive and persistent symptoms beyond just a low mood, significantly impairing daily functioning.”In other words, sadness can hurt and still let you live, depression doesn’t just hurt. It starts taking basic life functions hostage.
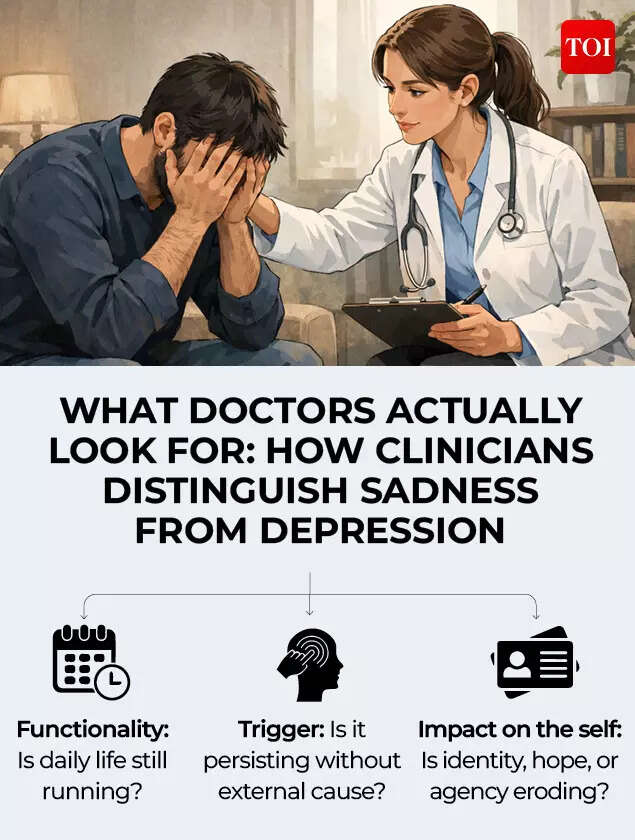
How clinicians distinguish sadness from depression.
“Depression as a clinical condition is a large mix of negative thinking pattern, disturbance in basic biological functions like sleep and appetite, inability to enjoy routine activities, and often lack of initiative and energy for daily routine tasks. Any such set of symptoms continuing beyond a period of two weeks, in the absence of any tangible external reason, and not amenable to one’s own efforts to pull oneself up, occurs owing to changes in brain chemistry,” explains Dr. Nimesh G Desai, senior consultant psychiatrist and former Director, IHBAS Delhi. Dr. Desai is not offering a calendar rule where sadness flips into depression after two weeks. He is describing when a sustained cluster of symptoms begins to look clinically concerning. Dr. Amit Sen, Director at Children First and a senior child and adolescent psychiatrist, cautions readers not to treat ‘two weeks’ as a universal switch. “The two-week cut-off for sadness to become depression is quite arbitrary,” he says. “In bereavement, sadness can last much longer but not cause the kind of damage or disability that depression can.”For clinicians, time and intensity are clues, not conclusions and the trouble begins when we turn either into a verdict. Dr. Barmi stresses that the difference between sadness and depression is frequently misunderstood. “Sadness and depression are not distinguished by intensity alone, but by function, duration, and impact on the self,” Dr. Barmi says. The real test is not how loud the pain feels, but what it starts to erode. “Sadness is a normal emotional state in response to day to day adverse life situations. Clinical depression is a disorder with definitive phenomenology and psychopathology. The difference lies in the duration, intensity, quality of emotional state and the associated psychophysiological symptoms,” observes Dr. Anandi Lal, Senior Director & HOD, Department of Mental Health & Behavioural Sciences, Max Super Speciality Hospital, Ghaziabad.
Dr. Anandi Lal
Describing sadness, Dr. Barmi places it firmly in the realm of difficult-but-viable days — the kind where life still runs, even if it runs heavier. “While sadness can be intense, it generally does not interfere with a person’s ability to maintain their daily responsibilities, work, or relationships for an extended period,” she says.In that space, the core of the self often stays intact — shaken, not shattered — and feeling low does not automatically erase the capacity to feel anything else. “A person experiencing sadness usually maintains their self-esteem. Individuals can still experience moments of pleasure, comfort, or happiness even when generally sad,” she says.
Cause and context: Sadness usually has a story, depression doesn’t
In clinical practice, what matters is whether the distress stays tethered to a clear life event and eases in waves over time, or persists beyond context in a way that signals a depressive disorder rather than ordinary sadness. “Sadness is a fundamental, healthy human emotion. It is a temporary feeling that occurs as a natural reaction to specific events, circumstances, or losses,” says Dr. Bhavna Barmi. In that frame, the emotion is not irrational; it is proportionate. “The intensity of the emotion correlates with the event, and the feeling generally fades over time as a person processes the situation,” she adds. Depression, she stresses, belongs to a different category altogether, not because it is ‘more intense’, but because it is not simply a reaction. “Clinical depression (major depressive disorder) is a recognized medical illness, not a temporary emotional state or a reaction to a single event,” Dr. Bhavna Barmi reflects. The causes are also rarely singular. “It is caused by a complex interplay of genetic, biological, environmental, and psychological factors,” she says. Dr. Mayher Barmi, Junior Resident, Department of Psychiatry, Swami Vivekanand Subharti University, elucidates that Major Depressive Disorder arises when pathological processes amplify symptoms beyond context-appropriate sadness.

Sadness vs. Depression: Triggers
Many treat depression as sadness that went on ‘too long’. Dr. Mayher Barmi argues that the relationship is more nuanced than the popular idea of sadness “turning into depression. “Depression is a distinct disorder that may be triggered by prolonged sadness, stress, loss, or vulnerability factors, but normal grief/sadness does not inherently ‘turn into’ depression,” she observes. The hinge, in her view, is whether the mind retains the ability to step back into life between the painful moments, or whether it begins to lose that capacity altogether. If the mind no longer finds its way back between difficult moments, clinicians grow more attentive to safety concerns including the possibility of suicide risk. “Depression is strongly associated with suicide risk, but in many cases, assessing that risk is a routine precaution rather than a sign of immediate danger. If treatment is underway and going well, most people and families do not need to be unduly alarmed about suicide risk,” observes Dr. Desai.
Symptoms that look alike, but behave differently
Sadness tends to move with the trigger and ease with time, while depression persists, dulls pleasure, and reshapes thought, energy, and self-worth. Dr. Mayher Barmi explains that in ordinary sadness, physical symptoms can appear, but they are usually mild, short-lived, and linked to the stressor. “An individual might feel mild tiredness, and a slight sleep-onset delay can occur, or there may be transient oversleeping after a bad day, but these typically improve as the trigger eases and functioning is largely preserved,” she says.She adds that appetite changes can be experienced briefly. “The appetite may decrease or increase for a few days revolving around the stressor, without marked weight change or significant preoccupation with diet,” Dr. Mayher Barmi says.
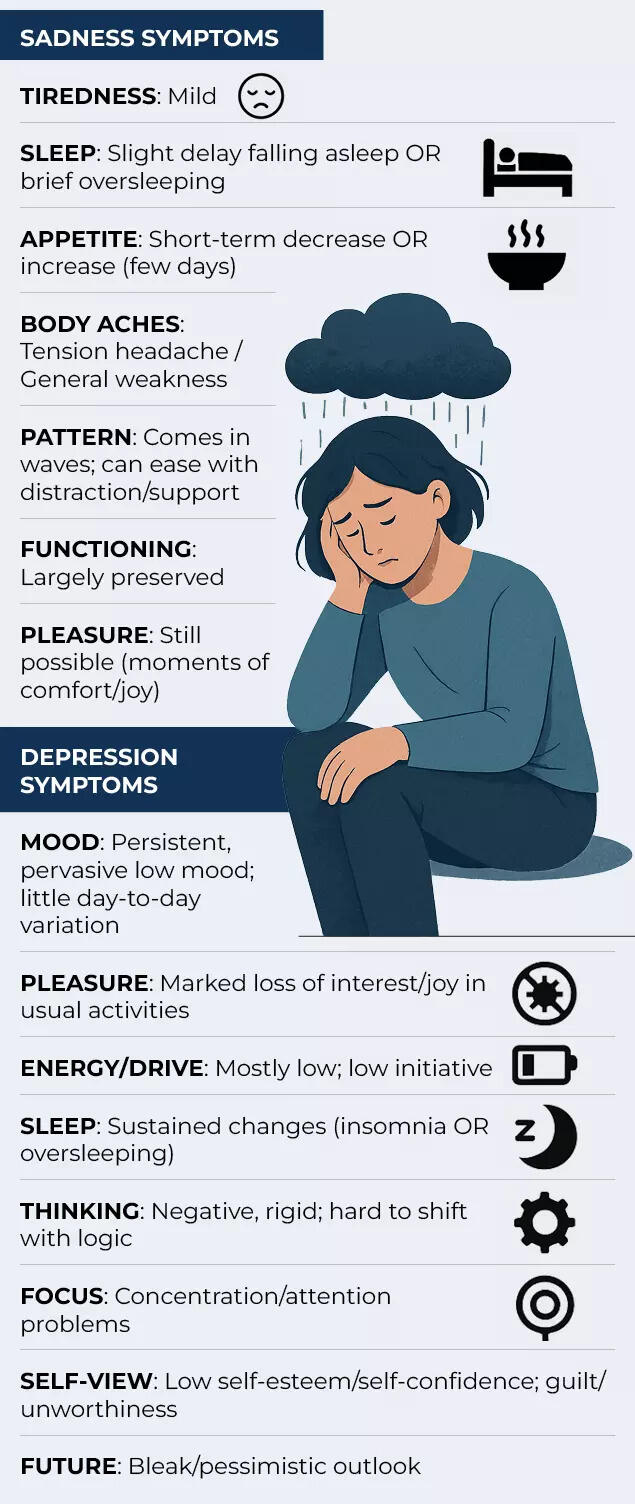
Sadness vs. Depression: Symptoms
Body aches can also show up during acute grief or distress, but they tend to fluctuate. “Somatic aches, such as a tension headache or generalized weakness, may appear during acute grief or distress, but they fluctuate and improve with distraction and social support,” she says.Depression, on the other hand, is marked by a deep loss of interest that goes beyond ordinary low mood. “The ability to derive pleasure or joy from previously enjoyable activities reduces significantly,” says Dr. Sen. He adds that this emotional shutdown is often accompanied by sustained depletion. “Energy levels and drive are mostly low,” he adds. Dr. Sen also points to a cognitive shift that is tough to understand. “Thoughts and perceptions change dramatically and do not respond to reason or logic,” he says.In depression, the mood does not behave like a passing reaction to life, it sits there with a stubborn consistency, regardless of what the day brings. Dr. Mayher Barmi puts it plainly, “The individual usually feels persistent and pervasive sadness, that varies little from day to day, and is often unresponsive to circumstances.”That emotional flattening is accompanied by deeper cognitive and self-perceptual changes. “Other symptoms include problems with concentration and attention, and decreased self-esteem and self-confidence,” Dr. Mayher Barmi says. Over time, the internal narrative hardens. “There are often ideas of guilt and unworthiness, along with bleak and pessimistic views of the future,” she adds.
The shared biology of sadness and depression
Sadness and depression differ in scale and persistence, but both can register biologically. What separates them is the depth, duration, and functional impact of those changes. “Depression is linked to changes across the brain and body,” Dr. Mayher Barmi says. She explains that these changes often begin at the level of brain chemistry. “Depression can affect the brain’s chemical messengers and the circuits they run on—systems involving serotonin, norepinephrine and dopamine,” she says.The impact also extends to key brain regions responsible for emotion, memory and regulation. “Brain areas such as the frontal cortex, hippocampus and amygdala can be structurally and functionally impacted,” Dr. Mayher Barmi cautions. Beyond the brain, depression can also disrupt broader bodily systems. “It may affect the neuroendocrine and immune system, contributing to neurotoxicity, reduced neurogenesis, and somatic comorbidity,” she adds.Biology is not exclusive to depression. Ordinary sadness and grief can leave temporary marks too. “Sadness and grief without clinical depression can produce measurable, usually time-limited biological changes in stress systems, sleep, immunity, and pain but these tend to be less severe, less persistent, and less functionally impairing,” Dr. Mayher Barmi says. In other words, grief can register in the body, but it typically does not hijack daily functioning in the way clinical depression does. She points out that bereavement-related research has documented short-term immune changes in the months after a loss, including reduced vaccine antibody responses, lower natural killer cell activity, and higher levels of systemic inflammatory markers.
Coping and care: What helps, what harms
In ordinary sadness, the first line of response is often simple and steady self-care. It is less about “snapping out of it” and more about keeping the system supported while life settles. “In normal sadness, following lifestyle changes are helpful: Exercise, yoga, pranayam, socialization, doing one’s work diligently, balanced diet without intoxicants and adequate sleep,” Dr. Lal says. He also flags the habits that can quietly deepen the slump. “Sedentary lifestyle, too much screentime, taking recourse to intoxicants, negative thought spiral are counter productive,” he adds.Most people manage routine sadness linked to external reasons or stressful life situations through familiar coping tools. “Generally, people deal effectively with regular sadness, for external reasons or stressful life situations with coping mechanisms like realistic problem solving and talking to family or friends. Healthy food and lifestyle, social and interpersonal activities, music or other such creative pursuits are equally helpful,” says Dr. Desai. The approach shifts when sadness crosses into clinical depression, and coping alone is no longer enough. “In clinical depression, a combination of positive lifestyle changes, therapy, and antidepressant medication results in a good therapeutic effect,” Dr. Lal says.
Naming sadness, recognising depression
Sadness, most of the time, is a visitor. It arrives with a reason, sits close for a while, and leaves traces—some tears, some sleepless nights, a tenderness that makes ordinary things feel heavier than they should. Literature has always given this kind of sadness a vocabulary and a storyline—something that can be carried, spoken, and gradually metabolised. Shakespeare’s line in Macbeth—“Give sorrow words”—rests on the idea that pain, when named, can begin to move. Medical science agrees that this is often true for ordinary sadness and grief: The feeling may hurt, but it usually remains tethered to context and still leaves room for relief, function, and return.Depression, however, is not simply sorrow with more volume. It is different in kind where the inner weather stops changing. Pleasure becomes illusive, sleep and appetite begin to shrink, thinking turns rigid and self-punishing, and daily functioning quietly collapses. That is why clinicians look beyond the story and towards the pattern: Duration, functional decline, and symptom clusters matter because depression behaves like a disorder, not a moment.Decoding the distinction is extremely crucial. If we label sadness as depression, we end up fearing what is human and often eased by time, support, and meaning. If we dismiss depression as “just sadness,” we delay assessment and care, sometimes until risk enters the picture. Our understanding of the difference tells us when to lean on coping and community and when to seek professional help.